You’ve tried everything. The calorie counting, the gym sessions, the latest diet trends. Yet the scale won’t budge, and you’re constantly battling bloating, fatigue, and cravings that feel impossible to control. Sound familiar?
The answer might not be in your willpower or workout routine—it could be hiding in your gut. More specifically, in something called increased intestinal permeability, commonly known as “leaky gut.” While it sounds like wellness jargon, the science behind how a compromised gut barrier affects your weight is compelling and increasingly well-documented.
In this article, we’ll explore the real connection between your digestive health and stubborn pounds, decode the warning signs your body is sending, and give you practical, research-backed strategies to heal from the inside out.
What Is Leaky Gut?
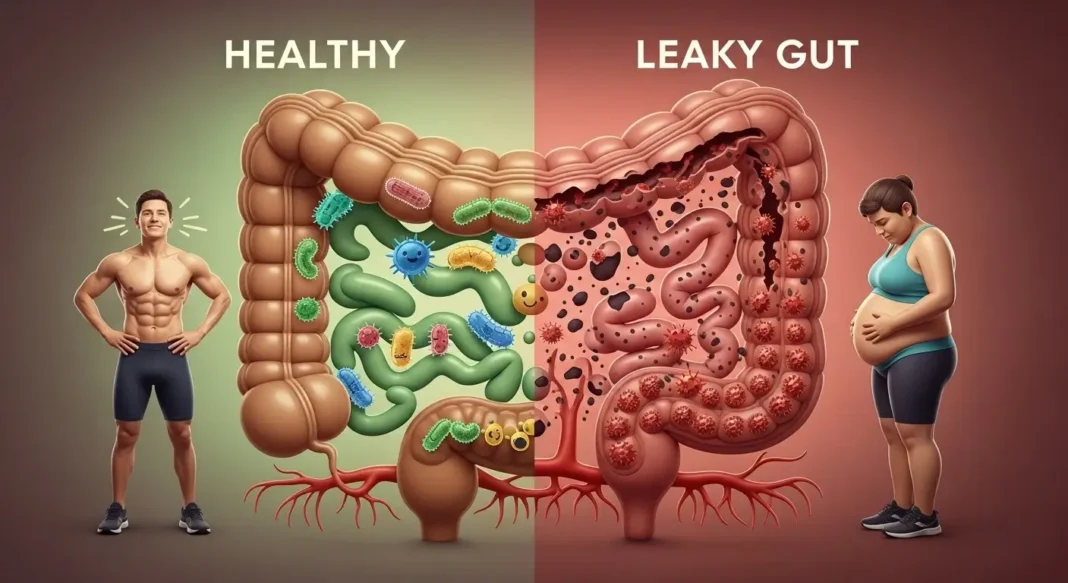
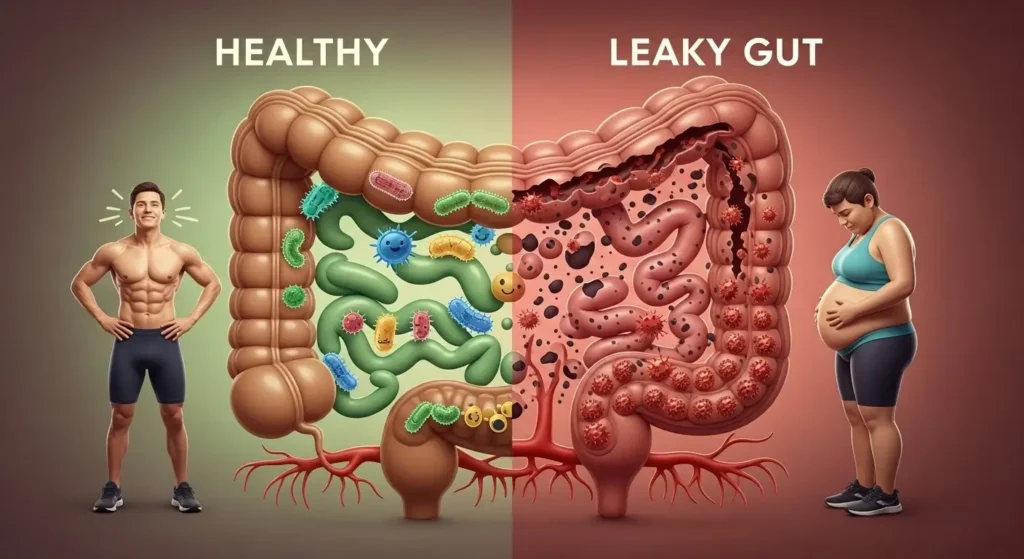
Your intestinal lining is one of your body’s most important barriers. Imagine a security gate that’s incredibly selective—it allows nutrients, water, and beneficial compounds to pass through while keeping toxins, bacteria, and undigested food particles out.
This selective barrier is just one cell thick and spans an area roughly the size of a tennis court, all folded up inside your abdomen. These cells are held together by proteins called tight junctions, which act like secure locks between each cell.
When everything’s working properly, this system is remarkably efficient. But when these tight junctions loosen—due to inflammation, poor diet, stress, or other factors—unwanted substances begin slipping through into your bloodstream. This is what we call increased intestinal permeability.
Your immune system recognizes these foreign invaders and launches an inflammatory response. It’s like your body’s alarm system going off repeatedly, and this chronic low-grade inflammation becomes the foundation for numerous health issues, including unexpected weight gain.
The Direct Answer: Yes, It Can
Here’s the truth: a compromised intestinal barrier absolutely can contribute to weight gain, and the relationship is more complex than simple calories in versus calories out.
When your gut lining is damaged, it triggers a cascade of metabolic disruptions. Your body shifts into constant defense mode, producing inflammatory molecules that interfere with how your cells respond to insulin. This makes it harder for your body to use glucose for energy, so it stores it as fat instead—particularly around your midsection.
The inflammation also disrupts the production and balance of hormones that control your appetite. Leptin, which signals fullness, stops working properly. Ghrelin, your hunger hormone, may increase. The result? You’re constantly hungry, never satisfied after meals, and craving exactly the inflammatory foods that perpetuate the problem.
Your metabolism slows down, your gut bacteria composition shifts toward species that extract more calories from food, and you develop food sensitivities that cause bloating and fluid retention. It’s not about willpower—your body’s fundamental metabolic processes have been compromised.
How This Actually Happens
Let’s break down the specific mechanisms:
Chronic Inflammation Changes Everything
When your gut barrier fails, inflammatory molecules flood your system. This isn’t the helpful acute inflammation that heals a cut—it’s persistent, systemic inflammation that affects every cell.
These inflammatory compounds interfere with insulin signaling, making your cells resistant. High insulin levels tell your body to store fat rather than burn it. Inflammation also triggers cortisol production, which promotes belly fat storage and increases cravings for comfort foods.
Think of inflammation as static on a radio—it disrupts all the clear signals your body needs to regulate weight effectively.
Your Hormones Fall Out of Balance
Beyond insulin resistance, damaged gut health wreaks havoc on your entire endocrine system:
Your brain stops receiving leptin’s “I’m full” signal, leading to overeating despite adequate energy stores. Cortisol stays chronically elevated, breaking down muscle and slowing metabolism. Your thyroid function can become impaired, further reducing your metabolic rate.
Nutrient Absorption Becomes Compromised
Even if you’re eating well, a damaged intestinal lining can’t effectively absorb essential nutrients. When your body lacks key vitamins, minerals, and amino acids, your metabolism slows because you don’t have the building blocks for efficient energy production.
You may experience intense cravings as your body desperately seeks missing nutrients. Poor protein absorption affects muscle maintenance, and since muscle burns more calories than fat, losing muscle mass further reduces your metabolic rate.
Your Gut Bacteria Change
Your microbiome plays a direct role in energy metabolism. When intestinal health deteriorates, the bacterial balance shifts, often favoring species that extract more calories from food and promote fat storage. These bacterial changes also affect how efficiently your cells produce energy.
Food Sensitivities Develop
As undigested food particles leak into your bloodstream, your immune system may begin producing antibodies against common foods. These reactions trigger inflammation, bloating, and fluid retention every time you eat the offending food—often without you realizing what’s happening.
Additionally, about 90% of your serotonin is produced in your gut. When gut health suffers, neurotransmitter production becomes disrupted, leading to increased cravings for comfort foods as your brain tries to boost feel-good chemicals.
Warning Signs to Watch For
Recognizing the symptoms early can help you address the issue before it becomes entrenched. Here are the most common indicators:
Digestive red flags:
- Persistent bloating, especially after meals
- Irregular bowel movements or alternating constipation and diarrhea
- Gas, abdominal discomfort, or acid reflux
- Undigested food visible in your stool
Systemic symptoms:
- Unexplained weight gain despite diet and exercise efforts
- Chronic fatigue or afternoon energy crashes
- Brain fog and difficulty concentrating
- Mood changes, anxiety, or depression
- Skin issues like acne, rosacea, or eczema
- Joint pain or muscle aches
Metabolic and appetite signals:
- Intense sugar or carbohydrate cravings
- Feeling hungry shortly after eating a full meal
- Difficulty managing blood sugar levels
- Feeling irritable or anxious when meals are delayed
Immune patterns:
- Frequent infections or seasonal allergies
- New food sensitivities developing
- Autoimmune conditions
You don’t need every symptom to have an issue. Even a few persistent signs, especially combined with stubborn weight, warrant attention.
What Causes This Problem?
Understanding the root causes helps you know what to address:
Dietary factors are often the biggest culprits. The standard Western diet—high in processed foods, refined sugars, and unhealthy fats—directly damages the intestinal barrier. Excessive sugar feeds harmful bacteria, while food additives like emulsifiers and artificial sweeteners compromise gut integrity.
Chronic stress is equally damaging. Your gut and brain communicate constantly, and stress hormones reduce blood flow to your digestive system, weaken the intestinal barrier, and alter bacterial composition. When stressed, your body deprioritizes digestion entirely.
Antibiotic overuse eliminates beneficial bacteria along with harmful ones. Even a single course can disrupt your microbiome for months, allowing opportunistic organisms to damage the intestinal barrier.
Infections like SIBO (small intestinal bacterial overgrowth), candida overgrowth, parasites, or H. pylori directly damage the intestinal lining or trigger inflammatory responses.
Regular alcohol consumption is directly toxic to intestinal cells, killing beneficial bacteria and impairing your liver’s ability to filter toxins.
NSAIDs like ibuprofen, when used regularly, reduce protective gut mucus and directly irritate intestinal cells.
Low fiber intake starves beneficial bacteria that produce compounds to nourish and protect your intestinal lining.
Who’s Most at Risk?
Certain people are more vulnerable:
Those with high-stress lifestyles, poor sleep quality, or sedentary habits face increased risk. People with autoimmune diseases, type 2 diabetes, or inflammatory bowel conditions are particularly susceptible. A history of frequent antibiotic use, especially in childhood, creates lasting vulnerability.
Dietary patterns matter enormously—diets high in processed foods and low in vegetables and fiber create the perfect environment for intestinal barrier breakdown.
How to Tell If Your Gut Is Behind Your Weight Struggles
Ask yourself:
- Do you experience bloating most days?
- Have you gained weight without changing your habits?
- Do you struggle to lose weight despite calorie restriction?
- Do you have intense cravings for sugar or carbs?
- Are you tired even after adequate sleep?
- Have you developed new food sensitivities?
- Do you feel hungry soon after full meals?
If several of these resonate, especially across different categories, addressing your digestive health could be transformative.
The Healing Protocol: A Step-by-Step Approach
Healing takes time and consistency, but it’s absolutely possible. Here’s how:
Step 1: Remove the Triggers
You can’t heal while continuing to damage your gut. Start by eliminating the most inflammatory foods for 3-4 weeks: gluten, dairy, sugar, processed foods, and alcohol. This isn’t forever—it’s a reset period.
Address chronic stress with daily practices like meditation, deep breathing, or nature walks. Even 10 minutes matters. Limit or eliminate NSAIDs and work with your doctor on alternatives.
Step 2: Support Your Digestion
Take a broad-spectrum digestive enzyme with meals to reduce the burden on your compromised system. Try diluted apple cider vinegar or lemon water before meals to support stomach acid production. And slow down—chewing thoroughly makes an enormous difference.
Step 3: Rebuild Your Microbiome
Include fermented foods like sauerkraut, kimchi, or kefir (if tolerated). Start with small amounts and gradually increase. Consider a high-quality multi-strain probiotic with at least 10-20 billion CFUs.
Feed your beneficial bacteria with prebiotic fibers from garlic, onions, asparagus, bananas, and oats.
Step 4: Repair the Lining
Consume bone broth daily—it’s rich in collagen and amino acids that nourish intestinal cells. Include omega-3 fatty acids from fatty fish, walnuts, or flaxseeds to reduce inflammation.
Eat zinc-rich foods like oysters, pumpkin seeds, and grass-fed beef. Include polyphenol-rich berries, green tea, and dark chocolate (85%+ cacao).
Step 5: Rebalance Your Lifestyle
Prioritize 7-9 hours of quality sleep—your gut lining regenerates during deep sleep. Move your body regularly with moderate exercise, but avoid excessive high-intensity workouts that stress the gut.
Stay hydrated with at least half your body weight in ounces of water daily. Continue daily stress management—this is non-negotiable.
Step 6: Be Patient
Most people notice improvements within 4-8 weeks, but complete healing typically takes 6-12 months depending on severity. Track symptoms, energy levels, and how your clothes fit rather than obsessing over the scale.
What to Eat and What to Skip
Emphasize these foods: Bone broth, fatty fish, fermented vegetables, leafy greens, berries, ginger, turmeric, coconut products, grass-fed meats, gluten-free whole grains, garlic, onions, and sweet potatoes.
Minimize or avoid: Gluten-containing grains, conventional dairy, refined sugar, processed foods with additives, artificial sweeteners, excessive alcohol, trans fats, factory-farmed meats, and regular NSAIDs.
Remember, this is a general guide. Your specific triggers may differ, so pay attention to how your body responds.
Supplements That May Help
While food should be your foundation, certain supplements have research supporting their use:
Probiotics can help recolonize beneficial bacteria. L-glutamine (5-15g daily) serves as fuel for intestinal cells. Zinc carnosine (75-150mg daily) supports barrier integrity. Collagen peptides (10-20g daily) provide gut-repairing amino acids.
Digestive enzymes reduce digestive burden while healing. Omega-3s (1000mg+ EPA/DHA) reduce inflammation. Vitamin D plays a role in immune function and barrier health.
Always consult a healthcare provider before starting supplements. Quality matters—choose reputable, third-party tested brands.
Timeline Expectations
Weeks 1-2: You might feel worse as your body adjusts. Stick with it.
Weeks 3-4: Many notice less bloating, more regular bowels, and improved energy.
Weeks 5-8: Digestion improves significantly. Cravings decrease. Some see the scale begin moving.
Months 3-6: As inflammation decreases, weight loss often accelerates. Skin, mood, and clarity continue improving.
Months 6-12: Deep healing continues. Food sensitivities may decrease, weight stabilizes at a healthier level.
Healing isn’t linear—expect some setbacks, especially when exposed to triggers.
Mistakes to Avoid
Don’t go too extreme with elimination diets—excessive restriction can reduce beneficial dietary diversity. Don’t over-supplement. Don’t expect overnight results or jump between protocols without giving them time.
Don’t ignore stress management—it’s essential, not optional. Don’t reintroduce trigger foods too quickly. Don’t focus only on diet while neglecting sleep, movement, and stress.
Address underlying infections like SIBO or candida—you won’t fully heal without treating them.
Real Stories
Sarah, 38, had gained 25 pounds over three years despite regular exercise. Testing revealed increased intestinal permeability and SIBO. After treating the infection, removing gluten and dairy, adding bone broth and fermented foods, and addressing work stress, she lost 15 pounds by month four without counting calories. A year later, she’d reached a healthy weight and maintained it effortlessly.
Michael, 45, worried he’d follow his dad’s path to diabetes when he started rapidly gaining weight. He simplified his approach: eliminated fast food, reduced alcohol, added vegetables to every meal, took a probiotic, and meditated for 10 minutes daily. Within two months, his heartburn disappeared. After six months, he’d lost 28 pounds and normalized his inflammatory markers.
Linda, 52, struggled with sudden weight gain during menopause. She discovered low stomach acid and multiple food sensitivities. By supporting digestion with apple cider vinegar, eliminating trigger foods, adding protein and fiber, and improving sleep, she healed her gut over four months and gradually lost 18 pounds.
These stories show there’s no one-size-fits-all approach, but healing is possible with consistency.
Frequently Asked Questions
Can you have this problem without digestive symptoms? Yes. Some people experience primarily systemic symptoms like fatigue, brain fog, or weight gain without obvious digestive issues.
Will healing automatically lead to weight loss? Not automatically, but as inflammation decreases and metabolism normalizes, many people naturally lose excess weight without additional restriction.
Can stress alone cause this? Yes, chronic stress significantly contributes to increased intestinal permeability through hormonal effects and reduced digestive function.
Are expensive tests necessary? Not always. Many people successfully heal by following general protocols and monitoring symptoms. If you’re not improving after several months, testing may provide useful insights.
Does everyone need to avoid gluten? Not permanently, but many benefit from temporary removal while healing. Some can reintroduce it later without problems.
How long before I see weight loss? Most people notice changes around 8-12 weeks as inflammation decreases, though timeline varies based on individual factors and consistency.
Can you drink coffee while healing? Moderate consumption (1-2 cups daily) is generally fine and may provide beneficial compounds. Listen to your body.
Will probiotics alone fix this? No. You must address root causes through diet, lifestyle, and stress management. Probiotics are one tool among many.
Final Thoughts
If you’ve been fighting unexplained weight gain alongside mysterious symptoms that doctors can’t quite pin down, your gut may be calling for help. The connection between intestinal permeability and weight is real, measurable, and—most importantly—addressable.
This journey isn’t a quick fix. It requires patience, consistency, and willingness to address multiple factors: what you eat, how you manage stress, your sleep quality, and how you support your body’s healing processes.
But the rewards extend far beyond the scale. People who heal their gut describe feeling like themselves again—energetic, clear-headed, and free from constant battles with cravings and inflammation.
Start where you are. Remove obvious triggers, add one or two supportive foods or practices, and commit to stress management. Track your symptoms, celebrate small victories, and remember that healing isn’t linear.
Your gut is remarkably resilient. Given the right conditions and enough time, it has an extraordinary capacity to heal. The weight you’ve been carrying may simply be your body’s response to inflammation and disruption. Address the root cause, and symptoms often resolve naturally.
You deserve to feel good in your body. Healing your gut might be the missing piece that finally makes everything click.
The information provided on HealthyPa.com is for educational and informational purposes only and is not intended as medical advice. The content on this website, including articles, reviews, and product recommendations, should not be used as a substitute for professional medical advice, diagnosis, or treatment.
Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or before starting any new supplement, diet, or exercise program. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
The statements regarding dietary supplements have not been evaluated by the Food and Drug Administration (FDA). These products are not intended to diagnose, treat, cure, or prevent any disease.
Individual results may vary. The testimonials and experiences shared on this website are individual cases and do not guarantee that you will achieve the same results.
If you are pregnant, nursing, taking medication, or have a medical condition, consult your healthcare provider before using any products reviewed or recommended on this site.
HealthyPa.com and its authors, contributors, and affiliated parties assume no responsibility for any consequences relating directly or indirectly to any action or inaction you take based on the information found on this website.
By using this website, you acknowledge and agree to this disclaimer.
HealthyPa.com is reader-supported. When you buy through links on our site, we may earn an affiliate commission at no additional cost to you. This helps us keep our content free and continue providing valuable health information. We only recommend products we genuinely believe in. Learn more in our full Affiliate Disclosure Policy.