Menopause 2025 Navigating the Revolution: Understanding the Health Transition That’s Finally Getting the Attention It Deserves
The conversation around menopause is experiencing a seismic shift in 2025. What was once whispered about behind closed doors is now being discussed openly in boardrooms, doctor’s offices, and social media platforms worldwide. With more than one billion women worldwide currently experiencing perimenopause, menopause, or postmenopause, and approximately 12% of the world’s population, or more than 1 million women, expected to reach menopause by 2025, this natural life transition is finally receiving the medical attention and societal recognition it deserves.
Gone are the days when menopause was viewed as a taboo subject or simply an inevitable decline. Instead, it can be understood as a new chapter—one of reflection, growth, and reinvention. As Generation X and millennials enter this phase of life, they’re reshaping how we understand, discuss, and treat this universal women’s health experience.
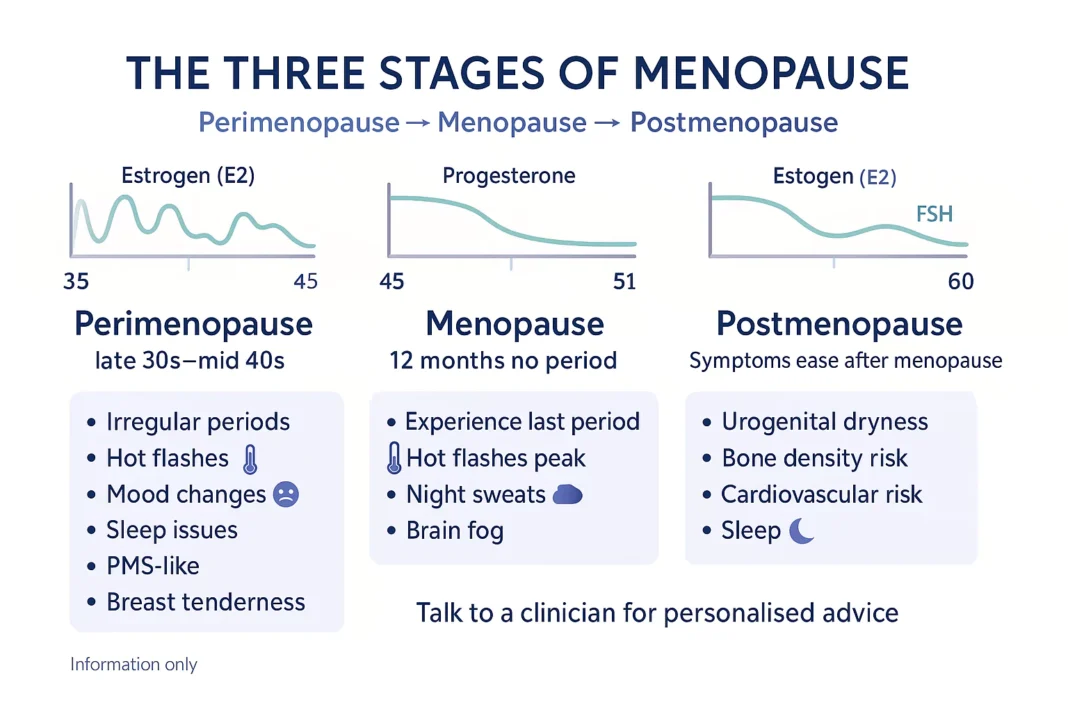
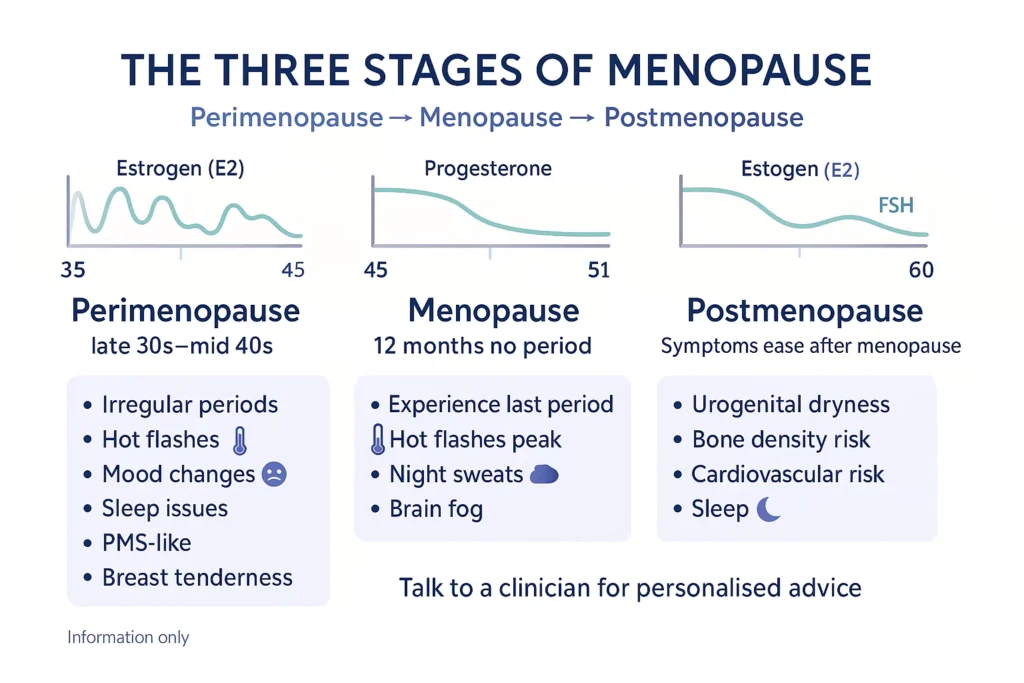
Understanding the Menopause Journey
Menopause isn’t a single event but rather a gradual process that unfolds over several years. Menopause is the permanent ending of menstruation, officially diagnosed when a woman has gone 12 consecutive months without menstruation. It typically occurs between the ages of 45 and 55, with 51 being the median age of natural menopause.
However, the journey begins much earlier during perimenopause, which means “around menopause” and represents the transitional period leading up to menopause. Perimenopause can begin eight to 10 years before menopause when your ovaries gradually produce less and less estrogen. This phase typically usually lasts about four years and typically starts in your mid-40s, though the timeframe can vary significantly among women.
The Three Stages Explained
Perimenopause: This is often the most challenging phase, characterized by fluctuations in hormones, which is why many people’s experiences can be inconsistent and rocky. During this time, women may experience irregular periods, with cycles becoming shorter or longer, and bleeding patterns changing dramatically.
Menopause: This is the definitive moment when periods have stopped for a full year. Unlike the other stages, menopause itself is a defined moment, so you don’t stay in this stage.
Postmenopause: The years following menopause, when many actually feel better as hormone levels stabilize at their new lower baseline.
The Wide Spectrum of Symptoms
One of the most frustrating aspects of the menopause transition is the sheer breadth of potential symptoms, many of which can be mistaken for other conditions. Rage, fatigue, mood swings, memory loss, hot flashes, itchy ears, inability to sleep, loss of libido, hair thinning, depression, weight gain, sore knees, night sweats, incontinence are all documented symptoms of perimenopause.
Vasomotor symptoms are experienced by almost 75% of women undergoing menopause, making hot flashes and night sweats among the most common complaints. However, the experience varies dramatically among individuals and across different demographic groups.
Understanding the Variations
Research reveals significant disparities in how different populations experience menopause. Black and Hispanic women, for example, tend to report more vasomotor symptoms, such as intense and more frequent hot flashes, than their white counterparts. Additionally, Black women in the U.S. tend to reach menopause a year earlier than white women or women of East Asian descent, and experience symptoms for up to 10 years—three years longer than the national average.
Beyond Physical Symptoms
The impact extends far beyond physical discomfort. Brain fog — Feeling forgetful during perimenopause is common, affecting cognitive function and professional performance. Many women describe experiencing new, seemingly random joint or muscle pain during perimenopause, while others struggle with significant mood changes and sleep disruptions.
The Economic Impact: A Hidden Crisis
The economic implications of inadequately managed menopause symptoms are staggering. The annual cost of menopause to national economies due to lost productivity, absenteeism, and premature exit from the labor force is substantial. Estimates range from annual costs of almost USD 2 billion in the UK to USD 1.8 billion in the U.S., USD 3.3 billion in Canada, USD 9.9 billion in Germany, and USD 12 billion in Japan.
This can lead to an overall loss of productivity and quality of life, making treatment crucial. Despite these significant costs, many women report feeling unsupported in the workplace during menopause, and menopause care remains inconsistent and highly dependent on a range of factors, from geographic location to health insurance coverage.
The Challenge of Diagnosis and Treatment
One of the biggest hurdles women face is getting proper recognition and treatment for their symptoms. Unlike menopause — defined by the cessation of menstruation — perimenopause can be sneaky and hard to pinpoint. There’s no one definitive test for it, and disentangling the symptoms from other factors can make it hard to treat.
Many women encounter dismissive attitudes from healthcare providers. As one woman shared: “They said, ‘You’re too young.’ It’s easy to discount the symptoms. Doctors will say ‘It’s just stress or whatever'”. This dismissal can lead to years of suffering and misdiagnosis.
Health care providers don’t usually recommend hormone level testing unless there is a medical reason to do so. This is because, for most women, hormone levels go up and down in an unpredictable way during the transition to menopause.
Finding the Right Care
General practitioners often aren’t afforded the time to thoroughly evaluate their patients for perimenopause. Specialists not only have more knowledge about this condition but are also not subject to the same time constraints. For women struggling to find appropriate care, The Menopause Society provides an online database of doctors who are trained and certified in treating menopause and perimenopause.
Treatment Options: A New Era of Possibilities
The landscape of menopause treatment has evolved significantly, moving beyond the one-size-fits-all approaches of the past. Personalized medicine is here. Some clinics now offer tailored treatments based on genetics, lifestyle, and biomarkers rather than treating all patients in the same ways.
Hormone Replacement Therapy: A Renewed Perspective
After years of hesitation, estrogen therapy is making a quiet return. Once sidelined due to early-2000s studies linking it to health risks, it’s now being reexamined—particularly for its benefits during and after menopause.
The key insight from recent research is timing. The problem with the patients in the two studies was they were far beyond the average age of becoming postmenopausal. Current evidence suggests that HRT can be valuable for certain women, particularly those who are healthy and closer to being postmenopausal.
Comprehensive Treatment Approaches
Modern menopause care goes beyond just hormone therapy. There are a variety of non-hormonal and hormonal interventions that can help alleviate symptoms of menopause. These include:
- Lifestyle modifications: There’s nothing that beats a healthy lifestyle. So, we should always start there
- Technology-assisted care: Advanced health-tracking wearables monitor everything from ovulation and menstrual cycles to sleep patterns and stress levels
- Complementary therapies: The use of infrared saunas and light therapy is becoming a go-to solution for women seeking natural ways to boost their recovery and cellular health
- Personalized nutrition: DNA-based insights are shaping wellness trends for women. Personalized nutrition plans can help people cope with allergies or intolerances, improve gut microbiome health, and support better digestion, immunity, and even mental clarity
The Growing Market and Awareness
The menopause market is experiencing unprecedented growth. The global menopause market size is projected to reach USD 27.63 billion by 2033, growing at a CAGR of 5.10% during the forecast period (2025–2033). This growth reflects increasing awareness and demand for solutions.
An increase in the number of menopause-related campaigns has increased awareness about it and related symptoms. Since 2009, globally, the 18th of October has been celebrated as World Menopause Day, while October is celebrated as a menopause awareness month.
Breaking Down Barriers and Stigma
Addressing stigma and improving education around menopause are essential for empowering women and improving their health outcomes. The silence surrounding menopause has historically prevented women from getting the care they need. Unfortunately, both awareness and access to menopause-related information and services remain a significant challenge in most countries. Menopause is often not discussed within families, communities, workplaces, or health-care settings.
However, this is changing rapidly. As Generation X and millennials ease into their 40s and 50s, they are ready to shake off the stigma around menopause and the time leading up to it — called perimenopause — in favor of embracing treatment.
Menopause as Empowerment and Reinvention
Rather than viewing menopause as decline, many women are embracing it as a period of transformation. This phase brings its share of challenges, but it also brings wisdom, perspective, and a sharpened sense of priorities. Many women describe a new clarity that allows them to make bold decisions and set firmer boundaries.
The data supports this perspective: A 2024 report by the Global Entrepreneurship Monitor noted that women aged 45 to 64 are one of the fastest-growing groups of new entrepreneurs in North America.
Looking Forward: Global Health Recognition
The importance of menopause as a global health issue is gaining recognition. The World Health Organization (WHO) has officially announced the theme of World Health Day 2025, “Healthy beginnings, hopeful futures,” which will focus on improving maternal and newborn health and survival, highlighting the continuum of women’s health needs throughout the lifespan.
The Global Alliance for Women’s Health was launched in 2024 to improve research, financing and advocacy for women’s health, securing $55 million in new funding to improve data, research and care delivery for women’s health in its first year alone.
Practical Steps Forward
For women navigating this transition, several key actions can help:
- Education and self-advocacy: Understanding the wide range of potential symptoms and knowing they’re not “all in your head”
- Finding specialized care: Seeking out healthcare providers trained in menopause medicine when possible
- Lifestyle optimization: Focusing on nutrition, exercise, sleep, and stress management
- Community support: Connecting with other women going through similar experiences
- Workplace advocacy: Pushing for menopause-friendly workplace policies and support
Conclusion: A New Chapter of Women’s Health
Janet Ko, founder of the Menopause Foundation of Canada, noted that “Women now spend up to half their lives in a stage of menopause, each with potential symptoms and long-term health risks that require proactive management. Recognizing it as a critical health transition is essential for effective policy and care”.
The menopause revolution of 2025 represents more than just increased awareness—it’s a fundamental shift in how we view women’s health across the lifespan. As research expands, treatments improve, and stigma decreases, women are finally getting the support they need during this significant life transition.
It is critical to see menopause as just one point in a continuum of life stages. By embracing this perspective and continuing to advocate for better care, research, and workplace support, we can ensure that the millions of women entering menopause in the coming years will have the resources they need not just to survive this transition, but to thrive through it.
The future of menopause care is bright, personalized, and empowering. As we move forward, the focus shifts from simply managing symptoms to optimizing health and supporting women in writing the next chapter of their lives with confidence and vitality.
Medical Disclaimer: This article is for informational and educational purposes only and is not intended as medical advice, diagnosis, or treatment. The information provided should not replace professional medical consultation, diagnosis, or treatment. Always consult with qualified healthcare professionals before making any decisions about your health, medications, or treatment plans. Individual experiences with menopause and perimenopause vary significantly, and what works for one person may not be appropriate for another. If you are experiencing symptoms that may be related to menopause or perimenopause, please consult with a healthcare provider who specializes in women’s health or menopause care. Never disregard professional medical advice or delay seeking treatment because of information you have read in this article.